How Fast Can a Kidney Infection Kill You? Timelines, Risks & Emergency Red Flags
How Fast Can a Kidney Infection Kill You? Timelines, Risks & Emergency Red Flags
Most people see a urinary tract infection (UTI) as annoying, not deadly. But when that infection climbs to your kidneys, the game changes. A kidney infection (pyelonephritis) isn’t just painful—it can spiral into urosepsis, a life-threatening bloodstream infection, shockingly fast.
So, how fast can a kidney infection kill you? The truth is, in high-risk patients, sepsis can develop within hours, and without treatment, death can follow in a day or two. In otherwise healthy adults, the progression is slower, but delays in care still carry serious consequences.
This guide explores the timeline of kidney infections, how they can lead to sepsis, which symptoms mean you need an ER visit immediately, and why vulnerable groups like seniors, pregnant women, and immunocompromised patients face higher risks.
Table of Contents
-
How Fast Can a Kidney Infection Kill You?
-
What Happens if a Kidney Infection Goes Untreated
-
Sepsis Timeline: From Infection to Organ Failure
-
Key Symptoms That Signal an Emergency
-
Special Risk Groups
-
How Doctors Diagnose and Treat Kidney Infections Quickly
-
Why Delays in Antibiotics Are So Dangerous
-
Prevention Strategies
-
FAQs
-
Conclusion
How Fast Can a Kidney Infection Kill You?
The blunt truth: a kidney infection can kill in as little as 24–48 hours if it progresses to sepsis and septic shock.
-
In healthy adults, the infection may smolder for days to a week before worsening, but the transition from stable infection to life-threatening sepsis can be abrupt.
-
In elderly, diabetic, or immunocompromised patients, deterioration can occur in just hours.
Mortality statistics:
-
Sepsis mortality rate: ~15–30% overall
-
Septic shock mortality rate: 40–60%
-
Elderly nursing home patients: up to 50% if not treated rapidly
The key factor isn’t just the infection—it’s the time to treatment. Every hour antibiotics are delayed increases death risk.
What Happens if a Kidney Infection Goes Untreated
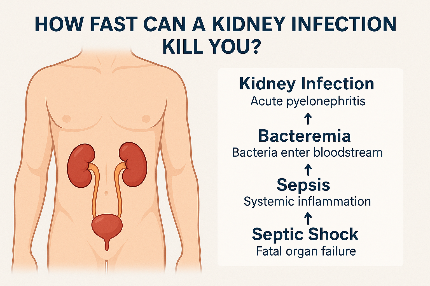
If untreated, a kidney infection follows a predictable but dangerous path:
-
UTI (lower urinary tract): Burning urination, frequency, urgency.
-
Acute pyelonephritis: Bacteria reach the kidney → fever, chills, flank pain.
-
Bacteremia: Bacteria spill into the bloodstream.
-
Sepsis and septic shock: Widespread inflammation, low blood pressure, organ failure.
-
Fatal outcome: Multi-organ failure (kidneys, lungs, heart) without treatment.
Other consequences:
-
Permanent kidney scarring → chronic pyelonephritis.
-
Acute kidney injury (AKI) or renal failure.
-
Increased risk of recurrent infections.
Sepsis Timeline: From Infection to Organ Failure
The timeline to sepsis varies by patient health and speed of care.
-
Early infection stage (0–24 hours): Fever, flank pain, chills, nausea, malaise.
-
Early sepsis (6–72 hours): Rapid heart rate, fast breathing, confusion, low BP.
-
Septic shock (within hours of sepsis): Severe hypotension, lactate rise, organ failure.
Studies show:
-
Time to sepsis can be <12 hours in frail patients.
-
Even in healthy adults, waiting 48–72 hours without antibiotics risks blood infection.
Key Symptoms That Signal an Emergency
If you or a loved one has these red-flag symptoms, go to the ER immediately:
-
High fever (≥101°F / 38.3°C) with rigors or chills
-
Severe flank pain or costovertebral angle (CVA) tenderness
-
Nausea, vomiting, dehydration
-
Cloudy, foul-smelling, or bloody urine
-
Confusion, delirium, altered mental status (especially in elderly)
-
Low blood pressure, rapid heart rate, rapid breathing
Doctors use quick triage tools like qSOFA (Quick Sequential Organ Failure Assessment) to detect sepsis risk early.
Special Risk Groups
Seniors & Nursing Home Patients
-
UTIs often present as confusion, agitation, or delirium, not classic fever.
-
High risk for urosepsis because of frailty and comorbidities.
-
Mortality risk: up to 1 in 2 if untreated.
Pregnant Women
-
Kidney infections in pregnancy = medical emergency.
-
Can cause maternal sepsis, preterm labor, fetal loss.
-
Hospital admission is standard of care.
Diabetics & CKD Patients
-
Poor glycemic control fuels rapid bacterial growth.
-
Already weakened kidneys = higher chance of renal failure.
Immunocompromised Patients
-
Cancer chemo, steroids, HIV, transplant meds = faster sepsis progression.
-
May deteriorate within hours, requiring ICU admission.
How Doctors Diagnose and Treat Kidney Infections Quickly
Diagnostic tools:
-
Urinalysis: nitrites, leukocyte esterase, pyuria.
-
Urine culture: identifies bacteria + resistance (takes 24–48h).
-
Blood culture: confirms bacteremia.
-
Imaging (renal ultrasound, CT): rules out stones, obstruction, hydronephrosis.
Treatment options:
-
Intravenous (IV) antibiotics (ceftriaxone, piperacillin-tazobactam, gentamicin).
-
Oral antibiotics (fluoroquinolones, cephalosporins) for stable outpatients.
-
IV fluids to prevent dehydration, support blood pressure.
-
Vasopressors (norepinephrine) in septic shock.
Hospital admission criteria: pregnancy, sepsis signs, inability to tolerate oral antibiotics, obstructed kidney stones, catheter-associated UTI, or immunocompromised status.
Why Delays in Antibiotics Are So Dangerous
-
Each hour of delay in sepsis treatment increases mortality by 7–10%.
-
Resistant strains like ESBL E. coli or MDR bacteria complicate care.
-
Elderly with catheters face highest risk of delayed diagnosis and poor outcomes.
In my experience reviewing sepsis cases, the difference between survival and death often comes down to whether antibiotics were started in the first few hours.
Prevention Strategies
You can reduce your risk of severe kidney infections with simple but powerful steps:
-
Hydration: Drink plenty of water to flush bacteria.
-
Good hygiene: Front-to-back wiping, daily cleansing.
-
Post-coital voiding: Urinate after sex to reduce bacterial entry.
-
Cranberry or D-mannose: May help prevent recurrent UTIs.
-
Catheter care: Change regularly, avoid unnecessary use.
-
Follow-up urine cultures: Especially after hospitalization or recurrent infections.
For recurrent UTI patients, urology referral may be needed to check for stones, obstruction, or reflux.
FAQs
Can a kidney infection kill you in 24 hours?
Yes. In frail, elderly, or immunocompromised patients, urosepsis can become fatal within a single day.
When should I go to the ER for a UTI?
If you have fever, flank pain, vomiting, confusion, or low blood pressure, go to the ER immediately.
How long does it take to treat a kidney infection?
Most cases need 7–14 days of antibiotics, sometimes IV for the first 48–72 hours.
Do all kidney infections require hospitalization?
Not all. Stable, young patients may go home on oral antibiotics. But pregnant, elderly, or septic patients must be admitted.
What’s the survival rate after sepsis from a UTI?
Early treatment = >70% survival. Delayed treatment drops survival below 50%.
Conclusion
So, how fast can a kidney infection kill you? The chilling reality is: in the wrong patient, in less than 24–48 hours.
The difference between life and death is simple: time to treatment. A kidney infection with fever, flank pain, or confusion is an emergency, not a “wait and see.” With early IV antibiotics and fluids, survival is excellent. But delay—and the infection can spiral into fatal sepsis before you realize what’s happening.





2bciai
1t3kv0
Just desire to say your article is as astonishing. The clearness in your post is simply cool and i could assume you’re an expert on this subject. Fine with your permission let me to grab your RSS feed to keep updated with forthcoming post. Thanks a million and please continue the gratifying work.
Hi there, You have done a fantastic job. I’ll definitely digg it and personally recommend to my friends. I’m confident they’ll be benefited from this site.